Ultrasonography – also known as ultrasound examination – is a simple, safe, and painless procedure that helps visualize organs and assess their structural makeup.
This method is used to diagnose many diseases in modern medicine.
Among them are various types of thyroid disorders.
What information do we get from an ultrasound examination of the thyroid gland?
When examining the thyroid gland, in addition to the organ itself, the surrounding neck structures are also examined.
The gland's size, structural uniformity, blood supply, the presence of focal changes – inclusions or nodules, their characteristics, as well as changes in nearby lymph nodes are evaluated.
In addition to the initial assessment, ultrasound examination also helps in the monitoring of already diagnosed pathology.
Along with the general assessment of the gland, it is especially important to describe the ultrasonographic characteristics of nodules if they are present.
It is based on the ultrasound evaluation that a decision is made on what the further management and monitoring plan should be in the case of a nodular goiter.
What do the medical terms that may appear in an ultrasound report mean?
Before visiting a doctor and receiving a final conclusion, unclear terms found in ultrasound results often cause confusion and anxiety in patients, especially when it comes to describing a nodular formation.
Therefore, in this article, we will discuss basic medical terms, their meaning, and possible interpretations, which will help you get a rough idea of what is happening in the structure of the thyroid gland before you see a doctor.
General description of the thyroid gland
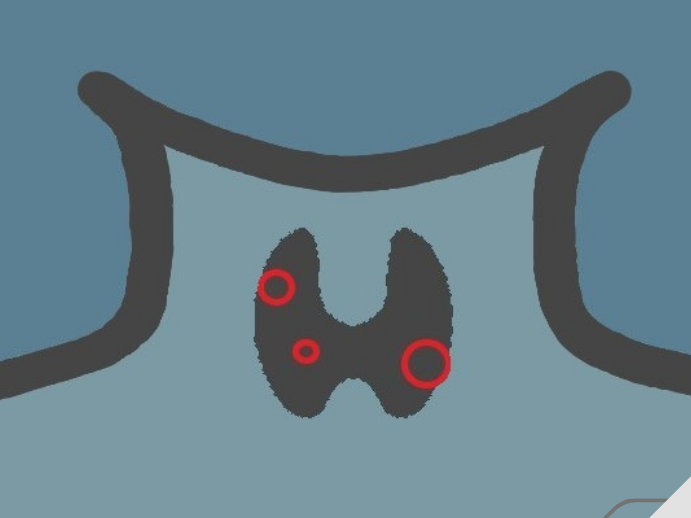
Here we find terms such as: left lobe, right lobe, and hyoid – also known as isthmus – which describe the anatomical structure of the thyroid gland.
It is a butterfly-shaped organ and consists of these three parts.
The isthmus or bridge connects the left and right lobes. Their size and characteristics are usually written separately in the conclusion.
Parenchyma – The tissue that makes up the thyroid gland is referred to as parenchyma.
Gland volume – The total volume should normally be less than 18 cm3 in women and less than 25 cm3 in men. The lower limit is not currently defined andIf the gland is functioning properly and responding to the body's demand for hormones, it is considered normal, even if its volume is small.
Changes in the gland can be diffuse or focal.
Diffuse – means that the process involves the entire gland evenly – for example, Diffuse goiter – describes a uniform enlargement of the gland in volume.
Focal changes may appear locally in the normal or altered parenchyma of the gland as a patch, area, or nodule. Unlike the latter, the area and patch do not have sharp boundaries – a contour.
Focal changes may include fibrotic areas or fibrotic ridges, indicating damage to the glandular tissue.
Echogenicity and Ecostructure
Echogenicity is the ability of tissues to reflect and reflect ultrasound waves, which are reflected on the ultrasound monitor by the device's transmitter during the examination process.
The echogenicity of different tissues in the body varies and is visualized on an ultrasound image as darker or lighter in color than the surrounding structures, which together create the organ's echostructure.
Hyperechogenic – i.e., a structure with increased echogenicity is lighter/lighter in color than the surrounding areas. In the case of a nodule, this description means that the risk of malignancy is minimal.
Hypoechogenic – i.e., a structure with low echogenicity appears darker. If a thyroid nodule is characterized as hypoechogenic, it has a relatively high risk of malignancy.
An anechoic structure, i.e., a structure devoid of echogenicity, is visualized as completely black. This is the most common characteristic of thyroid nodules, which are almost always benign.
Isoechogenic – when the structure does not differ in echogenicity from the surrounding areas.
As for the overall echostructure of an organ, it can be homogeneous or heterogeneous.
The echostructure of a normal thyroid gland should be homogeneous – that is, evenly uniform and bright.
And when structural changes are observed in the gland in the form of inclusions, areas, and nodes, this creates an alternation of uneven, different echogenicities in the image, and we say that the echostructure is heterogeneous.
Cystic, colloid, solid
You will encounter these terms when describing a node.
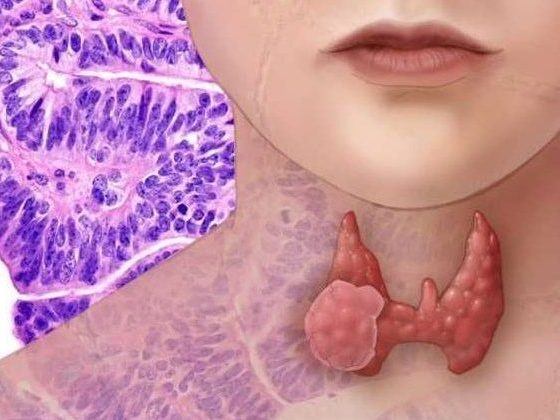
Thyroid nodules can be characterized as: colloid cyst, cystic nodule, solid nodule, mixed nodule, or solid-cystic nodule.
Colloid and cyst – means that the nodule is filled with fluid. A completely filled nodule in the thyroid gland is almost always benign and does not require biopsy for diagnostic purposes.However, if it grows too large and presses on the surrounding neck organs, it may be necessary to drain its contents/remove the fluid.
Solid – This description means that the nodule is entirely composed of tissue. The need for biopsy is determined by its additional characteristics.
Mixed structure or solid-cystic – This type of nodule in the thyroid gland contains both fluid and solid components. In some cases, additional evaluation of the tissue with a biopsy may be necessary.
Flake or spongy structure – when more than half of the volume of the nodule is occupied by multiple small (less than 5 mm) cystic inclusions (microcysts) that are separated from each other by thin septa.Most of these nodules are benign.
Calcification – Small (micro) calcifications in a nodule raise suspicion of malignancy, although they may simply be an indicator of the age of the nodule, especially if it is large.
Vascularization, Doppler
The term vascularization means blood supply.
Doppler ultrasound describes the nature of blood circulation in the gland as a whole and specifically in the nodule (if present).
This study, in combination with other data, helps the doctor to suspect various causes of hyperthyroidism and assess the risks of nodule malignancy.
Intense vascularization of a nodule may be indicative of malignancy, although benign nodules with the same characteristics are also frequently encountered.
Lymph node evaluation
When characterizing lymph nodes, attention is paid to: size and structure – whether its normal structure – the hilus – has been preserved.
Reactive lymph node – describes a lymph node that is enlarged in response to another process in the body, such as an infection or injury.
Suspicious signs that require attention are:
- Large size – more than 10 mm
- Presence of microcalcifications
- Enhanced vascularization
- Modified hilus.
Node Classification System – EU-TIRADS
It is important to emphasize that none of the features described above independently confirm the presence of malignancy.
Only with a combination of these signs can we suspect the malignancy of a nodule and, therefore, assign it to one of the following categories:
- Very low risk, low, medium or high risk nodes.
Accordingly, the next stage of diagnosis is planned - a biopsy.
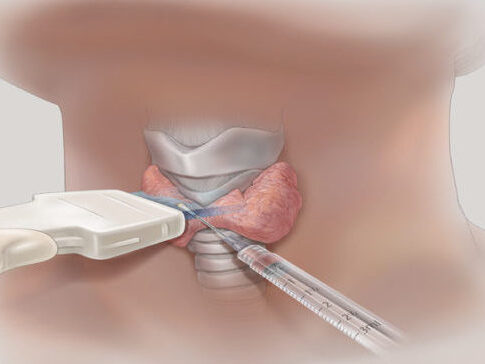
Fine needle aspiration biopsy is it A highly specific procedure that helps determine whether a nodule is benign or malignant.
It is the characteristics of the nodules that are summarized by the standardized classification system EU-TIRADS, which assesses the risk of malignancy of the nodule with scores from 1 to 5.
You will find this designation in the ultrasound report, and its interpretation is as follows:
EU-TIRADS 1: No nodular formation is detected.
EU-TIRADS 2: The nodule is benign, the risk of malignancy is 0%, and a biopsy is not required for diagnostic purposes.
EU-TIRADS 3: The nodule is low risk (risk of malignancy is 2-4%) – refers to oval-shaped, regular contours, iso- or hyperechoic nodules without suspicious features. Requires biopsy if its size is greater than 20 mm.
EU-TIRADS 4: The nodule is of intermediate risk (risk of malignancy is 6-17%) – refers to an oval-shaped, regular-contoured, hypoechoic nodule without suspicious features. Biopsy is required if its size is greater than 15 mm.
EU-TIRADS 5: The nodule is high-risk (risk of malignancy is 26-87%) – refers to a nodule with suspicious features such as: non-oval shape, irregular contour, presence of microcalcifications, and markedly decreased echogenicity.A biopsy is required if it is larger than 10 mm, although in smaller cases a biopsy may be considered or more frequent monitoring may be planned.
Author: Elga Giorgadze (MD of Endocrinology)
Continue reading: